Abstract
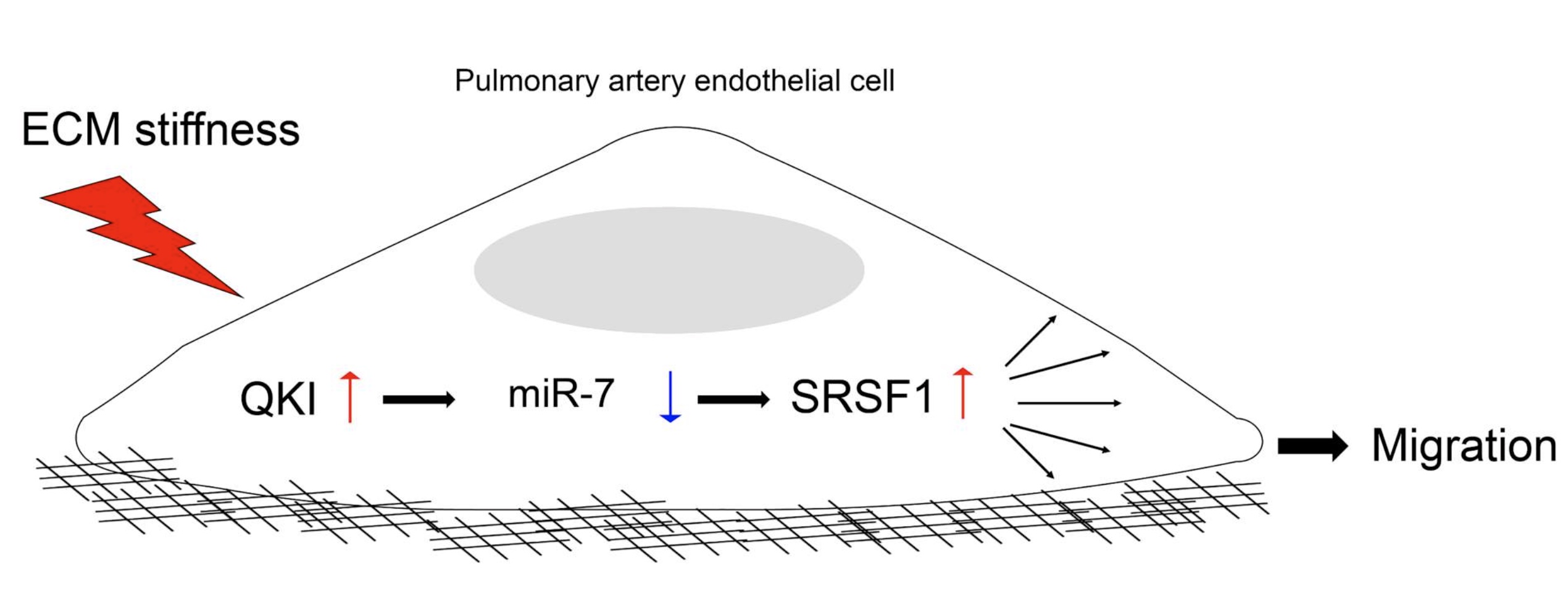
Pulmonary arterial hypertension (PAH) refers to a set of heterogeneous vascular diseases defined by elevation of pulmonary arterial pressure (PAP) and pulmonary vascular resistance (PVR), leading to right ventricular (RV) remodeling and often death. Early increases in pulmonary artery stiffness in PAH drive pathogenic alterations of pulmonary arterial endothelial cells (PAECs), leading to vascular remodeling. Dysregulation of microRNAs can drive PAEC dysfunction. However, the role of vascular stiffness in regulating pathogenic microRNAs in PAH is incompletely understood. Here, we demonstrated that extracellular matrix (ECM) stiffening downregulated miR-7 levels in PAECs. The RNA binding protein Quaking (QKI) has been implicated in the biogenesis of miR-7. Correspondingly, we found that ECM stiffness up-regulated QKI, and QKI knockdown led to increased miR-7. Downstream of the QKI-miR-7 axis, the serine and arginine rich splicing factor 1 (SRSF1) was identified as a direct target of miR-7. Correspondingly, SRSF1 was reciprocally up-regulated in PAECs exposed to stiff ECM and was negatively correlated with miR-7. Decreased miR-7 and increased QKI and SRSF1 were observed in lungs from PAH patients and PAH rats exposed to SU5416/hypoxia. Lastly, miR-7 upregulation inhibited human PAEC migration, while forced SRSF1 expression reversed this phenotype, proving that miR-7 depended upon SRSF1 to control migration. In aggregate, these results define the QKI-miR-7-SRSF1 axis as a mechanosensitive mechanism linking pulmonary arterial vascular stiffness to pathogenic endothelial function. These findings emphasize implications relevant to PAH and suggest the potential benefit of developing therapies that target this miRNA-dependent axis in PAH.